Understanding Thermoplastic Attributes in Clinical Splinting
This article focuses on the core attributes of thermoplastic splinting materials.
Thermoplastics are a foundational material in hand therapy and occupational therapy. They are used daily to fabricate splints that protect healing tissues, restore function, manage deformity, and support rehabilitation across acute and chronic conditions. Despite their widespread use, thermoplastics are often discussed in brand terms rather than material attributes. This can obscure meaningful differences and lead to suboptimal material selection.
This article focuses on the core attributes of thermoplastic splinting materials. It is intended to help clinicians make more informed decisions by understanding how material properties influence fabrication, fit, comfort, durability, and clinical outcomes.
Thermoplastic Attributes:
Activation temperature refers to the temperature range at which the material becomes pliable. Most clinical thermoplastics activate between approximately 60°C and 70°C.
Materials with lower activation temperatures are often preferred for patients with fragile skin, reduced sensation, or acute inflammation. Lower temperatures reduce the risk of burns and allow closer direct molding on the patient.
Higher activation temperatures can provide a firmer working window and may reduce unintended stretching during fabrication. However, they require greater care during handling.
Activation temperature should always be considered in relation to patient presentation and clinical environment.
Working time is the duration the material remains moldable after removal from the heat source. Longer working time allows for more detailed contouring, particularly in complex anatomical areas such as the thumb web space or ulnar border of the hand.
Shorter working time can be advantageous when rapid fabrication is required or when the therapist wants the material to set quickly once positioned.
Working time is influenced by material thickness, ambient temperature, and the method of heating. Clinicians should match working time to their fabrication style and the complexity of the splint design.
Resistance to stretch describes how much the material elongates when tension is applied during molding. This attribute is critical for maintaining consistent thickness and predictable fit.
Materials with low resistance to stretch can thin excessively if pulled during molding. This may lead to weak points, pressure areas, or loss of structural integrity over time.
Higher resistance to stretch provides greater dimensional stability. These materials are often preferred for splints requiring precise alignment or load bearing support.
Understanding stretch behavior helps prevent over thinning and improves long term splint durability.
Memory refers to the material tendency to return to its original flat shape when reheated. High memory materials attempt to revert strongly, while low memory materials retain their molded form more readily.
High memory materials are useful when remolding is anticipated. They allow repeated reshaping without accumulating distortion. This is particularly valuable in serial splinting or evolving conditions.
Low memory materials hold their shape firmly once molded. This can be advantageous when long term form retention is required and frequent remolding is unlikely.
Memory should be matched to the expected course of treatment rather than viewed as universally positive or negative.
Rigidity describes how stiff the material is once cooled. This attribute directly affects the level of support the splint provides.
High rigidity materials are suitable for immobilisation, fracture management, and tendon protection where minimal movement is required.
Lower rigidity materials allow controlled movement and may be more appropriate for dynamic splinting or functional support.
Rigidity is influenced by material composition, thickness, and design geometry. Thicker materials naturally increase rigidity, but material choice remains a key factor.
Conformability refers to how well the material adapts to anatomical contours without excessive pressure. Drape describes how smoothly the material settles over curves when molded.
Materials with good conformability improve patient comfort and reduce pressure points. This is especially important in areas with bony prominences or compromised soft tissue.
High drape materials allow gravity assisted molding with minimal force. This can improve precision and reduce fabrication time.
Poor drape may require more manual pressure and increases the risk of uneven thickness or discomfort.
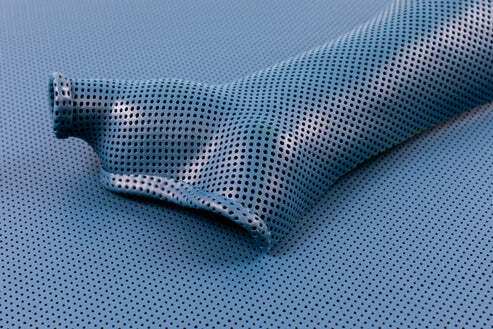
Surface texture plays a significant role in patient tolerance. Smooth materials reduce friction and are easier to clean. Textured or perforated materials improve breathability and moisture management.
Perforations can enhance comfort in long term wear and in warm climates. However, they may slightly reduce overall strength and require careful edge finishing.
Surface finish should be selected based on wear duration, skin condition, and hygiene considerations.
Thickness affects strength, rigidity, and weight. Thinner materials are lighter and less bulky but may lack sufficient support for certain applications.
Thicker materials provide greater strength but can reduce comfort and dexterity. In some cases, strategic reinforcement or layered designs offer a balance.
Therapists should consider thickness as part of a system rather than a standalone choice.